Navigation
Aromatherapy and Hair Loss
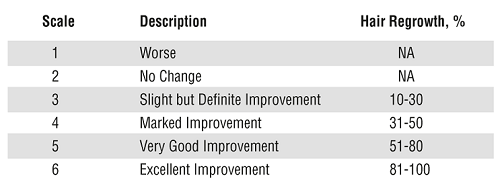
Abstract Objective To investigate the efficacy of aromatherapy in the treatment of patients with alopecia areata. Design A randomized, double-blind, controlled trial of 7 months' duration, with follow-up at 3 and 7 months. Setting Dermatology outpatient department. Participants Eighty-six patients diagnosed as having alopecia areata. Intervention Eighty-six patients were randomized into 2 groups. The active group massaged essential oils (thyme, rosemary, lavender, and cedarwood) in a mixture of carrier oils (jojoba and grapeseed) into their scalp daily. The control group used only carrier oils for their massage, also daily. Main Outcome Measures Treatment success was evaluated on sequential photographs by 2 dermatologists (I.C.H. and A.D.O.) independently. Similarly, the degree of improvement was measured by 2 methods: a 6-point scale and computerized analysis of traced areas of alopecia. Results Nineteen (44%) of 43 patients in the active group showed improvement compared with 6 (15%) of 41 patients in the control group (P=.008). An alopecia scale was applied by blinded observers on sequential photographs and was shown to be reproducible with good interobserver agreement (κ=0.84). The degree of improvement on photographic assessment was significant (P=.05). Demographic analysis showed that the 2 groups were well matched for prognostic factors. Conclusions The results show aromatherapy to be a safe and effective treatment for alopecia areata. Treatment with these essential oils was significantly more effective than treatment with the carrier oil alone (P=.008 for the primary outcome measure). We also successfully applied an evidence-based method to an alternative therapy. Complete Aromatherapy and Alopecia Study With the recent resurgence of interest in alternative medicine, aromatherapy (aroma, from the Greek meaning spice) has attracted great public interest in its health-promoting or medicinal properties. As with other forms of alternative medicine, scientific bases for the claims made are few,2 - 3 but in dermatologic studies, physiological and psychological benefits were found after treatment of psoriasis with aromatherapy.4 Significant, consistent improvement in behavior occurred in 1 of 4 patients with dementia5 in 10 repeated experiments. Aromatherapy is also useful in hospice care.6 As examples of proven therapeutic benefit, use of sandalwood oil has been shown to significantly inhibit skin papillomas in mice.7 Tea tree oil is an effective bacteriocide8 and fungicide, especially for Malassezia furfur.9 Use of essential oils can also alter the barrier functions of the skin10 and induce contact dermatitis.11 Cedarwood, lavender, thyme, and rosemary oils have hair growth–promoting properties. These oils have been anecdotally used to treat alopecia for more than 100 years. To date, there have been no controlled trials to evaluate this treatment. Our experience using aromatherapy provides anecdotal evidence that several patients have had marked improvement with this form of therapy. Our aim in this study was to test the hypothesis that pharmacologically active stimulants for hair growth are present in these oils and that use of these oils can be therapeutic in patients with alopecia. Alopecia areata is a common condition affecting 1% of the Western world. It can cause substantial social and psychological distress and is often highly detrimental to the patient's well-being and self-esteem. In 1 study,12 patients with alopecia areata had an increased risk of developing a psychiatric illness. An autoimmune cause is widely accepted. However, it is thought that stress can affect its course. Current conventional treatments have limited success or unacceptable toxic effects. The course of alopecia areata is unpredictable, but factors affecting prognosis are well established. A poor prognosis is indicated by the long duration of the condition (>1 year), associated autoimmune conditions (eg, thyroid disease), atopy, and family history.13 - 16 Patients Eighty-four patients were randomized into 2 groups by the aromatherapist (M.J.). All patients signed a written consent form before the trial. The trained aromatherapist explained how to use the oils and demonstrated the technique of scalp massage. The oils were massaged into the scalp for a minimum of 2 minutes. A warm towel was then wrapped around the head to aid absorption of the oils. Patients were advised to use this technique every night. There were 2 arms to the trial. The active group received the essential oils: Thyme vulgaris (2 drops, 88 mg), Lavandula agustifolia (3 drops, 108 mg), Rosmarinus officinalis (3 drops, 114 mg), and Cedrus atlantica (2 drops, 94 mg). These oils were mixed in a carrier oil, which was a combination of jojoba, 3 mL, and grapeseed, 20 mL, oils. The control group received the same carrier oils without added essential oils, and the oils were identical except in smell, which could not be mimicked in the control. Measurement and Evaluation Initial and 3- and 7-month assessments were made by 3 methods: 1. A 4-point scale, such as that described by MacDonald Hull and Norris,17 was used to check that the severity was similar in active and control groups, as follows: 1 indicates vellus hair or no hair; 2, sparse pigmented or nonpigmented terminal hair; 3, terminal regrowth with patches of alopecia areata; and 4, terminal regrowth in all areas. 2. A standardized professional photographic assessment of each volunteer was taken at the initial interview and after 3 and 7 months. Changes in these photographic assessments formed the primary outcome measure, with improvement as the most important factor. These changes were scored independently by 2 dermatologists (I.C.H. and A.D.O.) who were unaware of the therapy administered. Improvement in photographic assessment was graded using a numerical scale (Figure 1). Figure 1. The scale used in the photographic assessment to measure changes in hair growth after intervention with active essential oils compared with the control. NA indicates not applicable. 3. A further secondary outcome measure was performed. A map was traced onto transparent film wherever the alopecia occurred in patches. These tracings were then transferred onto flat acetate sheets. A computerized image analyzer was used to calculate the areas of alopecia at the initial assessment and after 3 and 7 months. Statistical Methods We calculated that if improvement occurred in 20% more patients with active treatment than in the control group it would require 47 active and 47 control patients to detect improvement at a 5% significance level with a power of 80%.18 Statistical analysis was performed on an intention-to-treat basis. A pooled variance estimate Student t test for independent samples was used to test improvement in the patients' alopecia with the map-tracing method. The χ2 test was used to detect improvement in the active and control groups. A Mann-Whitney U test, corrected for ties, was used to assess the significance of the degree of improvement in scored photographic assessment. The level of agreement of the alopecia scoring scale between 2 assessors was examined using the Cohen weighted κ statistic. The trial was approved by the Joint Ethical Committee for the Grampian Health Board and by the University of Aberdeen, Aberdeen, Scotland. Results Eighty-four patients entered the trial; 28 (68%) of the patients in the control group and 35 (81%) of the patients in the active group completed the trial (Figure 2). The patients were well matched for the important demographic indicators that might affect response to therapy (Table 1). The distribution of patients by the 4-point scale was similar in both groups. Figure 2. Flow diagram showing the randomization of patients to the active and control groups. The improvement was statistically significant in all assessments undertaken. The primary outcome measure of improvement vs no improvement showed improvement with essential oils (P=.008, χ2) (Table 2). The degree of improvement shown in the photographs was assessed by the Mann-Whitney U test and was significant (P=.05). The results of the alopecia scale, which scored the degree of improvement (from 1-6), are illustrated in Figure 3. The measurement of traced areas, which could be performed in only 32 patients, showed a mean±SD reduction in area affected of 103.9 ± 140.0 cm2 compared with −1.8 ± 155.0 cm2 in the control group (Figure 4). This was significant, with P =.05 (Student t test). A relative risk of 2.6 (95% confidence limits, 1.2, 5.6) was calculated for the likelihood of improving on the active therapy. Weighted κ statistic was 0.84 for agreement between scorers on the assessment of the photographic scale, showing good interrater correlation. Figure 3. Results of the photographic assessment of the degree of improvement in alopecia on a 6-point scale (see Figure 1). Figure 4. Results of computerized analysis of traced areas of alopecia in active and control groups. Bars indicate SD. This indicates that this is a reproducible method of assessment. One patient who received active treatment and had an excellent response (ie, a score of 6 on our scale) is pictured in Figure 5. Figure 5. A patient showing an excellent response (6 on the scoring scale) to essential oil therapy. This indicates that this is a reproducible method of assessment. One patient who received active treatment and had an excellent response (ie, a score of 6 on our scale) is pictured below. Comment The responses were variable but showed a clear and statistically significant advantage to treatment with this standardized regimen of aromatherapy. Although the tradition of aromatherapy is to combine several oils, it seems likely that 1 of these agents has a stimulatory effect on hair growth. One male patient also had severe androgenic alopecia, which was not included in the assessment of efficacy, and within this area there was some moderate regrowth of hair and improvement in alopecia areata. There was a higher dropout rate in the control group, which could be explained by the fact that the volunteers became discouraged with the 7-month protocol. The control oil was not odorless because the carrier oils have some smell, and patients did not know what aroma to expect. However, they may have surmised that their treatment was inactive and withdrew from the trial. The control group's relative lack of response again suggests a pharmacoactive property of the topically applied therapy as opposed to an effect arising from the comforting, relaxing effect of massage and of the application procedure, which was the same for both groups. Previous studies of alopecia therapies have used only subjective scales of improvement, such as those described by MacDonald Hull and Norris.17 We found these scales less helpful because there are large intervals between the points in the alopecia scale. We validated the method of sequential photography with a standardized approach using a professional photographer's studio. Images were judged by blinded observers and showed good agreement. This proved to be the most blinded and unbiased approach because there was no possibility of smelling which treatment had been applied. We encountered no significant adverse events from this treatment, which makes the therapeutic ratio high compared with other therapies, such as diphencyprone,14 ,16 squaric acid dibutylester,19 and systemic or intralesional corticosteroid injections. Populations in other trials may differ in prognostic factors. Shapiro et al20 and Gordon et al14 found a 38% success rate in producing cosmetically acceptable regrowth in patients with alopecia using diphencyprone. A review of psoralen–UV-A therapy for alopecia areata by Taylor and Hawk21 revealed that phototherapy was disappointing, with minimal benefit. Therefore, this aromatherapy trial, with an improvement rate of 44%, is comparable to and possibly of more benefit than trials of conventional therapies for alopecia areata. Compared with these other treatments, its safety is also greater, offering a better therapeutic ratio. References 2 Vickers A. Yes, but how do we know it's true? knowledge claims in massage and aromatherapy. Complement Ther Nurs Midwifery. 1997;363- 65 3 Martin GN. Olfactory remediation: current evidence and possible applications. Soc Sci Med. 1996;4363- 70 4 Walsh D. Using aromatherapy in the management of psoriasis. Nurs Stand. 1996;1153- 56 5 Brooker DJ, Snape M, Johnson E, Ward D, Payne M. Single case evaluation of the effects of aromatherapy and massage on disturbed behaviour in severe dementia. Br J Clin Psychol. 1997;36287- 296 6 Welsh C. Touch with oils: a pertinent part of holistic hospice care. Am J Hosp Palliat Care. 1997;1442- 44 7 Dwivedi C, Abu-Ghazaleh A. Chemopreventive effects of sandalwood oil on skin papillomas in mice. Eur J Cancer Prev. 1997;6399- 401 8 Hammer KA, Carson CF, Riley TV. Susceptibility of transient and commensal skin flora to the essential oil of Melaleuca alternifolia (tea tree oil). Am J Infect Control. 1996;24186- 189 9 Nenoff P, Haustein UF, Brandt W. Antifungal activity of the essential oil of Melaleuca alternifolia (tea tree oil) against pathogenic fungi in vitro. Skin Pharmacol. 1996;9388- 394 10 Yamane MA, Williams AC, Barry BW. Terpene penetration enhancers in propylene glycol/water co-solvent systems: effectiveness and mechanism of action. J Pharm Pharmacol. 1995;47978- 989 11 Weiss RR, James WD. Allergic contact dermatitis from aromatherapy. Am J Contact Dermat. 1997;8250- 251 12 Koo YM, William VR, Shellow MD, Hallman CP, Edwards JE. Alopecia areata and increased prevalence of psychiatric disorders. Int J Dermatol. 1994;33849- 850 13 van der Steen PHM, van Baar HMJ, Happle R, Boezeman JMB, Perret MJ. Prognostic factors in the treatment of alopecia areata with diphencyprone. Am Acad Dermatol. 1991;24227- 230 14 Gordon PM, Aldridge RD, McVittie E, Hunter JAA. Topical diphencyprone for alopecia areata: evaluation of 48 cases after 30 months' follow up. Br J Dermatol. 1996;134869- 871 15 De Prost Y, Paquez F, Touraine R. Dinitrochlorobenzene treatment of alopecia areata. Arch Dermatol. 1982;118542- 545 16 Weise K, Kretzschmar L, John SM, Hamm H. Topical immunotherapy in alopecia areata: anamnestic and clinical criteria of prognostic significance. Dermatology. 1996;192129- 133 17 MacDonald Hull S, Norris JF. Diphencyprone in the treatment of long standing alopecia areata. Br J Dermatol. 1988;119367- 374 18 Pocock SJ, Hughes MD. Estimation issues in clinical trials and overviews. Stat Med. 1990;9657- 671 19 Frattasio A, Germino M, Cargnello S, Patrone P. Side-effects during treatment with SADBE. Contact Dermatitis. 1997;36118- 119 20 Shapiro J, Tan J, Ho V, Tron V. Treatment of severe alopecia areata with topical diphenylcyclopropenone and 5% minoxidil: a clinical and immunopathologic evaluation. J Invest Dermatol. 1995;104(suppl 5)36S 21 Taylor CR, Hawk JLM. PUVA treatment of alopecia areata parrialis, totalis and universalis: audit of ten years' experience at St. John's Institute of Dermatology. Br J Dermatol. 1995;133914- 918 Author Information Accepted for publication April 16, 1998. The Soropotomists International of Aberdeen, Scotland, provided financial support for the trial.Aromatherapy for hair loss
With herbalism as its basis, aromatherapy involves the use of essential oils and essences derived from plants, flowers, and wood resins, which are generally massaged into the skin. These essential oils have been used to complement traditional medicine with some benefit.1
Eighty-six patients diagnosed as having alopecia areata were invited to take part in this randomized, controlled trial. These patients were interviewed, and they completed a questionnaire. Patients with a medical history of hypertension, epilepsy, or pregnancy were excluded. Two of 86 patients were excluded because they had androgenic alopecia. Topical medication and intralesional corticosteroid therapy for the alopecia were discontinued before the trial.






1 Whitmore SM, Leake NB. Complementary therapies: an adjunct to traditional therapies. Nurse Pract. 1996;2110- 13
We thank Jill Mollison, BSc, for statistical advice and the members of the Aberdeen Alopecia Self Help Group for their participation.
Corresponding author: Isabelle C. Hay, MRCP, Department of Dermatology, Ward 48, Aberdeen Royal Infirmary, Foresterhill, Aberdeen AB25 2ZN, Scotland (e-mail: ad.ormerod @ abdn.ac.uk).
